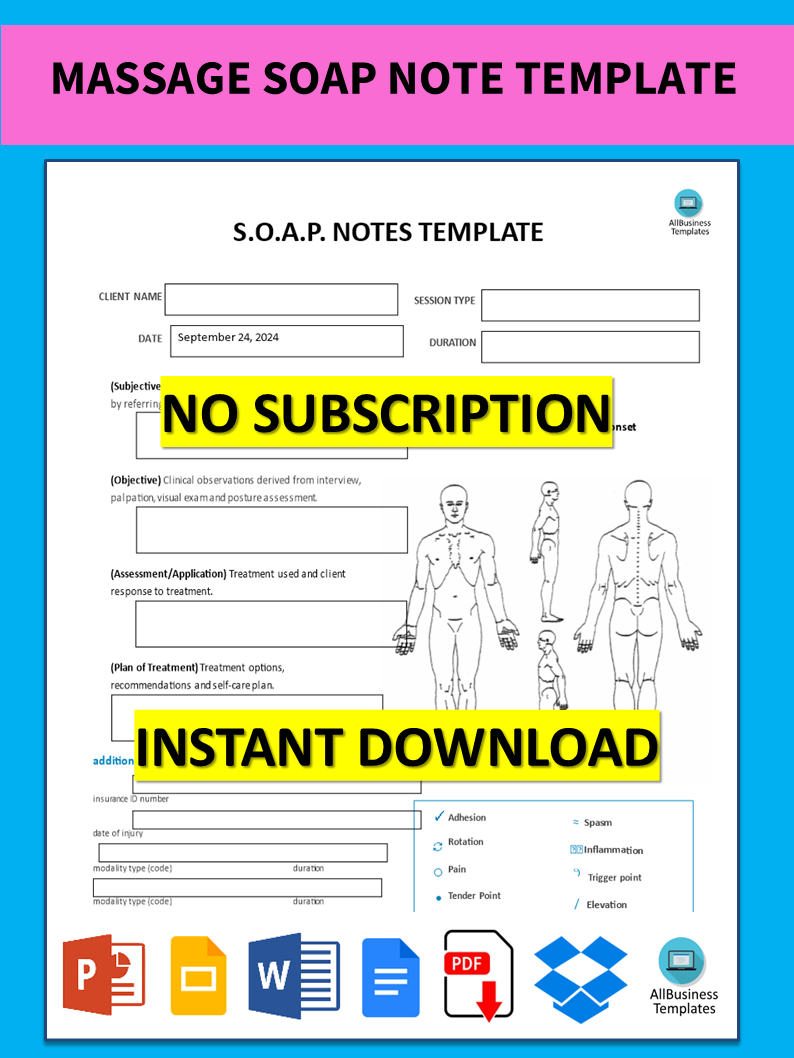
Massage Soap Note
Save, fill-In The Blanks, Print, Done!
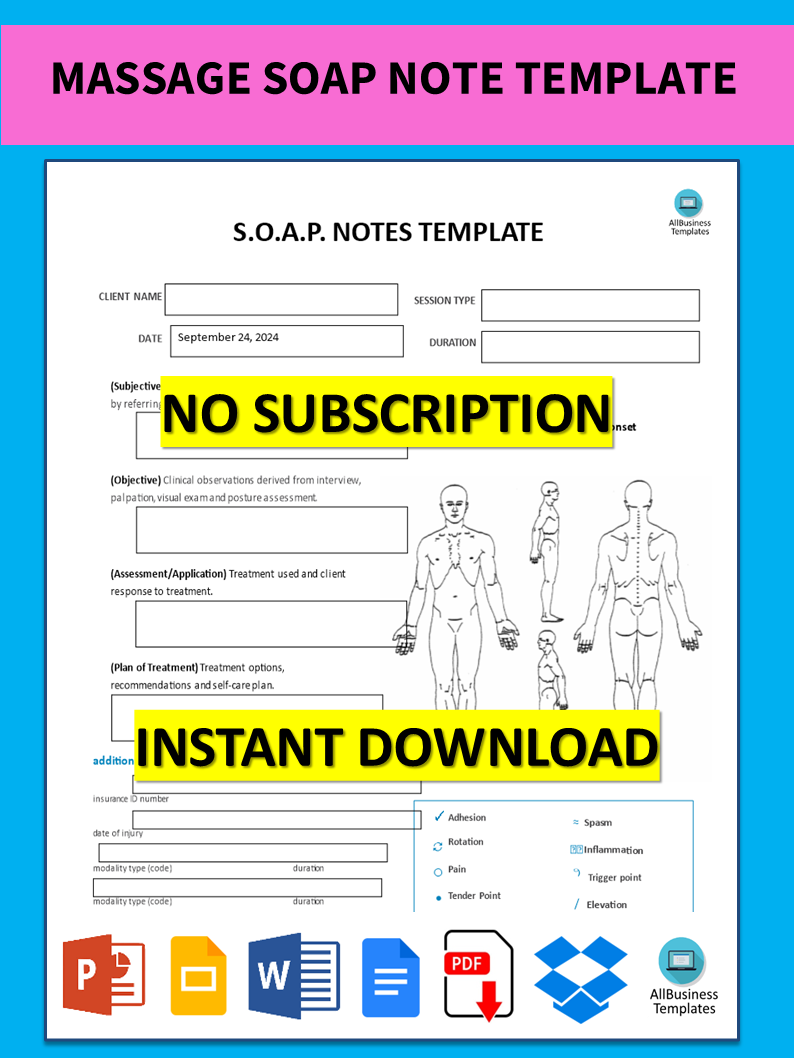
Download Massage Soap Note
Microsoft Word (.docx)Or select the format you want and we convert it for you for free:
- This Document Has Been Certified by a Professional
- 100% customizable
- This is a digital download (89.95 kB)
- Language: English
- We recommend downloading this file onto your computer.
What is the use of a SOAP Note in massage therapy? What benefits do they pose to clients and therapists? Our template was created to assist you in recording client information, types of messages received, and any subsequent notes. It is very user-friendly and can be tailored to meet your requirements.
SOAP notes for massage therapy are an essential part of keeping the client records intact, tracking their improvement over a certain period, and most importantly ensuring that there is continuity of care. They also assist in speaking to other health professionals if required and give proper evidence of treatment attended.
Massage SOAP notes are universal objective criteria utilized by massage therapists to document the details of the client and the treatment rendered. The acronym SOAP means Subjective, Objective, Assessment, and Plan, which captures all relevant details about the client's status and treatment as well as the plan for the client.
Here’s a breakdown of each section:
- Subjective (S): This portion encompasses the client’s account of the situation and symptoms alongside the history of the condition. More often the section captures the client's feelings, experiences, and complaints as expressed in their own words. For example:
- "Client reports lower back pain after lifting heavy objects."
- "Client feels tension in the shoulders and neck."
- Objective (O): In this segment, the therapist presents quantifiable and can be seen data. It incorporates physical assessments like:
- Degrees of movement range
- Evaluation of posture
- Tightness or tenderness of a muscle that can be felt
- Assessment (A): This section describes a therapist's evaluation of a client, formed from both subjective and objective facts. It may include:
- Analyzing muscle imbalance to select appropriate treatment
- Identification of any potential problem areas
- Evaluation of progress relative to previous sessions in the form of progress notes.
- Plan (P): This particular section of the paper indicates treatment strategies and recommendations for a given client. It covers the following:
- Explanation of the various massage techniques that were applied,
- The number of future sessions: their frequency and duration,
- Tasks or self-care instructions are given to the client.
Using this S.O.A.P. notes template guarantees you will save time, cost, and effort! It comes in Microsoft Office format and is ready to be tailored to your personal needs. Completing your document has never been easier!
In case Google Docs is your preferred option, simply click on 'Open with Google Docs' at this moment or download right away our example massage soap note template in Word format!
DISCLAIMER
Nothing on this site shall be considered legal advice and no attorney-client relationship is established.
Leave a Reply. If you have any questions or remarks, feel free to post them below.
SOAP Note Templates
How do you write a good SOAP note? What does SOAP stand for? Download these SOAP note templates directly.
Read moreLatest templates
Latest topics
- Excel Templates
Where do I find templates for Excel? How do I create a template in Excel? Check these editable and printable Excel Templates and download them directly! - GDPR Compliance Templates
What do you need to become GDPR compliant? Are you looking for useful GDPR document templates to make you compliant? All these compliance documents will be available to download instantly... - Google Docs Templates
How to create documents in Google Docs? We provide Google Docs compatible template and these are the reasons why it's useful to work with Google Docs... - IT Security Standards Kit
What are IT Security Standards? Check out our collection of this newly updated IT Security Kit Standard templates, including policies, controls, processes, checklists, procedures and other documents. - Letter Format
How to format a letter? Here is a brief overview of common letter formats and templates in USA and UK and get inspirited immediately!
cheese