HTML Preview Clinical Progress Note page number 1.
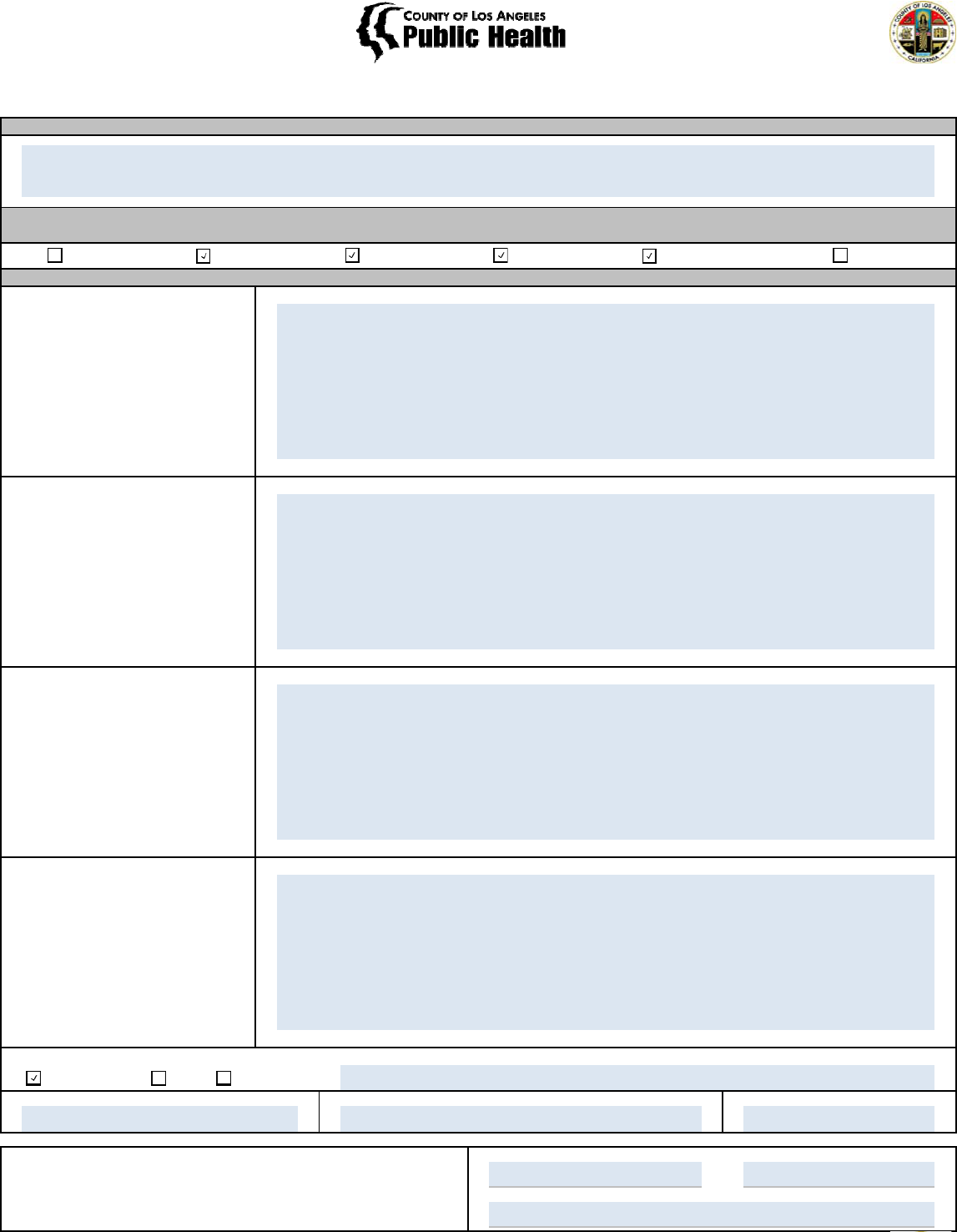
Dimension 1 Dimension 2 Dimension 3 Dimension 4 Dimension 5 Dimension 6
S - Subjective:
O - Objective
A - Assessment
P - Plan
If the patient's preferred language is not English, were linguistically appropriate services provided?
Not Applicable Yes No, Please Explain:
Provider Name: Provider Signature: Date:
Client Name: Medi-Cal ID:
Treatment Agency:
ASAM DIMENSION(S)
Please choose the dimension(s) that this note addresses
SOAP FORMAT
SUBSTANCE ABUSE PREVENTION AND CONTROL
PROGRESS NOTE (SOAP FORMAT)
DSM-5 DIAGNOSIS(ES)
1/28/2016Greg Lollipop
Greg Lollipop
Client reported feeling depressed, but not suicidal, since his bike accident and stated “I didn’t care if I was sad with the
pills or smack.” He stated, “I don’t believe in treatment, but I’ll give it a try as long as I have help with the cravings.” He
reported being fearful of relapse due to strong cravings, but stated “I feel better being on Suboxone, it makes the
cravings more manageable.” He reported residual pain from his bike accident.
Client was withdrawn and guarded. He participated in group therapy and engaged in the group process with the help of
the counselor. He was able to identify two “triggers,” such as “seeing the scars from my accident” and “being around
other people who use stuff.” Withdrawal symptoms have resolved; however, he still has strong cravings despite
improvement since starting Suboxone.
Observable data or information supportin
g
the subjective statement. This may include
the ph
y
sical appearance of the patient (e.
g
.,
sweaty, shaky, comfortable, disheveled,
well-groomed, well-nourished), vital signs,
results of completed lab/diagnostics tests,
and medications the patient is currently
taking or being prescribed.
Patient statements that capture the theme
of the session. Brief statements as quoted
by the patient may be used, as well as
paraphrased summaries.
The counselor’s or clinician’s assessment
of the situation, the session, and the
patient’s condition, prognosis, response to
intervention, and progress in achieving
treatment plan goals/objectives. This may
also include the diagnosis with a list of
symptoms and information around a
differential diagnosis.
The treatment plan moving forward, based
on the clinical information acquired and
the assessment.
Opioid Use Disorder: Severe
Opioid use: post-withdrawal. Overall, Mr. Doe appears engaged in SUD treatment at this time. He still has strong
cravings and is fearful of relapse, but appears to be responding to Suboxone. Unclear if higher dose is necessary – will
coordinate with Suboxone prescriber. He continues to report depressive and pain symptoms and would benefit from
further mental and physical health follow up, respectively.
Substance Use
- Client will continue IOP and MAT as prescribed. He agreed to attend at least 1 Narcotics Anonymous meeting at least
1x per week. Continue Suboxone and coordinating with Suboxone prescriber.
- Counselor will refer the client to case management for help with housing and employment.
Mental Health
- Given ongoing depressive symptoms, will refer for mental health assessment.
Physical Health
- Client will call his PCP to make an appointment by next week.
- Refer to case management to f/u to ensure the client made PCP appointment.
123-45-6789
This confidential information is provided to you in accord with State and Federal laws and regulations including but
not limited to applicable Welfare and Institutions Code, Civil Code and HIPAA Privacy Standards. Duplication of
this information for further disclosure is prohibited without the prior written authorization of the patient/authorized
representative to who it pertains unless otherwise permitted by law.
John Doe
Healing SUD Treatment Center
Progress Note Template Revised 04/13/2016