SOAP Note Example templates
What is the format for SOAP notes?
SOAP is an acronym for Subjective, Objective Assessment and Plan, which is a method of documentation common in the health and healthcare industry. SOAP Notes are therefore often considered a clinical document used in many healthcare organizations. This resource discusses the audience and purpose of the SOAP specification, suggested content for each section, and examples of appropriate and inappropriate language.
SOAP Notes are a common way for healthcare and other teams to organize the information they need to share with each other as they collaborate or pick up where others left off. SOAP annotations should be clear, well-written, and easy to understand so your team can find the information they need.
A good SOAP description should help healthcare professionals better document, retrieve, and apply detailed information about a specific case, thereby improving the quality of patient care.
-
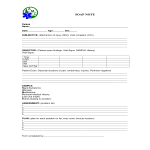
Medical Soapnote
How to create a Soap Note? This medical soap note covers the most important topics, such as: signs, symptoms, allergies, medications, pertinent medical history, last oral intake, events leading to the accident.
View template -
Blank Soap Note
How to create a Soap Note? What is the format for SOAP notes? Download this Blank Soap Note template now for your own benefit!
View template -
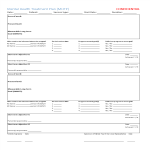
Mental Health Treatment Plan
What are the steps involved in writing a mental health treatment plan? Why is mental health treatment necessary? Download our template now and get started today!
View template
Latest topics
- GDPR Compliance Templates
What do you need to become GDPR compliant? Are you looking for useful GDPR document templates to make you compliant? All these compliance documents will be available to download instantly... - Google Docs Templates
How to create documents in Google Docs? We provide Google Docs compatible template and these are the reasons why it's useful to work with Google Docs... - IT Security Standards Kit
What are IT Security Standards? Check out our collection of this newly updated IT Security Kit Standard templates, including policies, controls, processes, checklists, procedures and other documents. - Letter Format
How to format a letter? Here is a brief overview of common letter formats and templates in USA and UK and get inspirited immediately! - Google Sheets Templates
How to work with Google Sheets templates? Where to download useful Google Sheets templates? Check out our samples here.