Notas de SOAP de masaje plantillas, contratos y formularios.
How to create a Massage SOAP Note and what does S.O.A.P. mean?
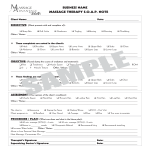
A Massage SOAP Note is a standardized documentation tool used by massage therapists to record client information and treatment details. SOAP stands for Subjective, Objective, Assessment, and Plan, providing a structured way to capture relevant information about a client's condition, the treatment provided, and the future course of action.
Using a Massage SOAP Note:
Subjective (S): This section includes the client's own description of their condition, symptoms, and any relevant history. It often captures the client’s feelings, experiences, and complaints in their own words. For example:
- "Client reports lower back pain after lifting heavy objects."
- "Client feels tension in the shoulders and neck."
Objective (O): This section contains measurable and observable data gathered by the therapist. It includes physical findings, such as:
- Range of motion measurements
- Postural assessments
- Palpable muscle tightness or tenderness
Assessment (A): This section is the therapist's professional evaluation of the client's condition based on the subjective and objective information. It may include:
- Analysis of muscle imbalances
- Identification of potential problem areas
- Progress notes comparing previous sessions
Plan (P): This section outlines the treatment plan and any recommendations for the client. It includes:
- Details of the massage techniques used
- Frequency and duration of future sessions
- Homework or self-care advice for the client
Massage SOAP notes are crucial for maintaining accurate client records, tracking progress over time, and ensuring continuity of care. They also help in communicating with other healthcare professionals if needed and provide legal documentation of the treatment provided.
Using this SOAP note template guarantees you will save time, cost, and effort! It comes in Microsoft Office format and is ready to be tailored to your personal needs. Completing your document has never been easier!
Download this Massage SOAP Note template now for your own benefit!