Massage Soap
Speichern, ausfüllen, drucken, fertig!
What does SOAP mean when taking notes? How to draft Massage Soap notes? Download this Massage Soap template now!
Verfügbare Gratis-Dateiformate:
.pdf- Dieses Dokument wurde von einem Professional zertifiziert
- 100% anpassbar
Business Unternehmen Life Privat note Hinweis Client Klient Pain Schmerzen Notes Anmerkungen Sample Note Beispiel Hinweis Soap Note SOAP notiz Massage Upper Oberer, höher Massage Soap Note Massage SOAP Hinweis massage soap note template for excel massage soap note template massage SOAP notes Massage SOAP Notizen
What does SOAP mean when taking notes? How to draft Massage Soap notes?
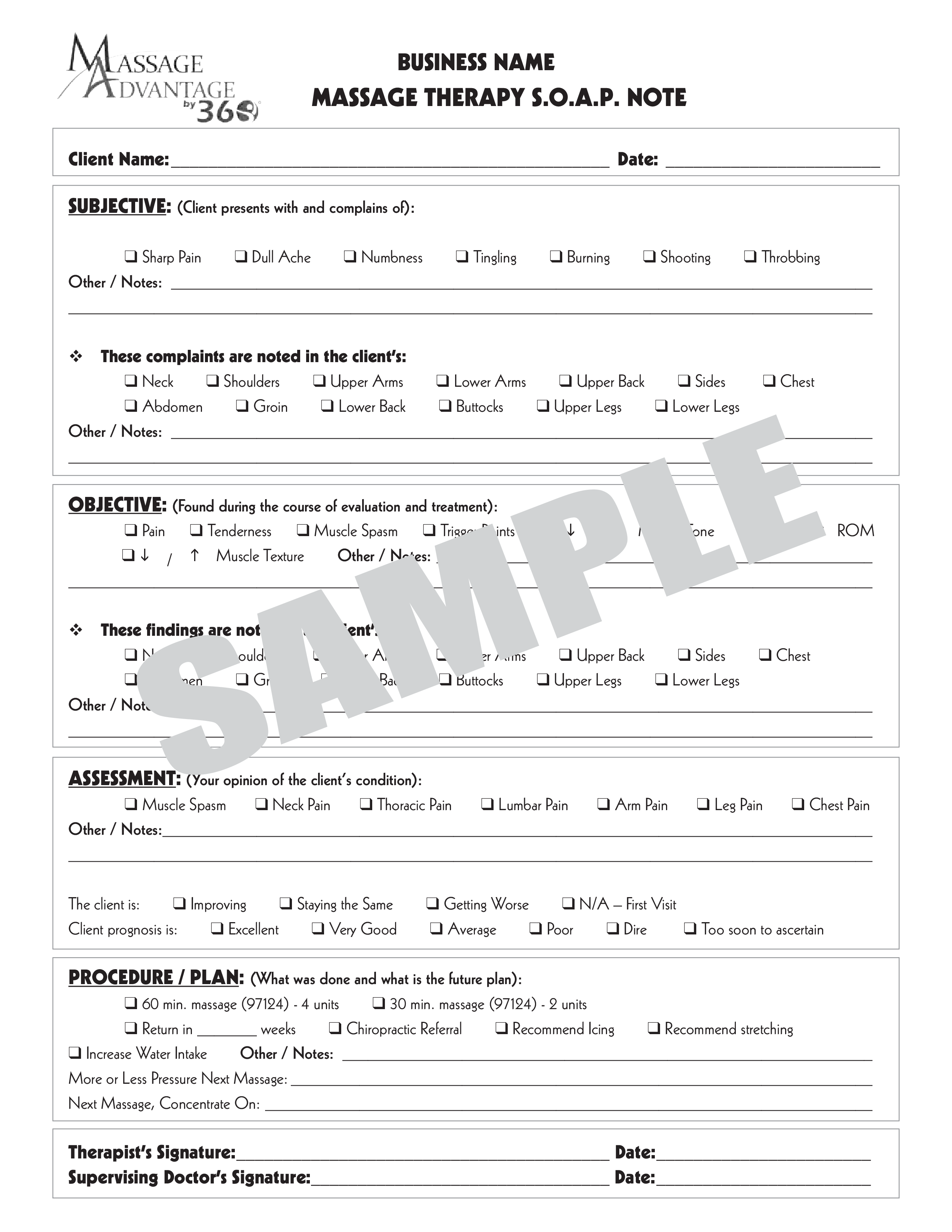
Massage SOAP notes are standardized documentation used by massage therapists to record client information and treatment details. SOAP stands for Subjective, Objective, Assessment, and Plan, and it provides a structured way to capture relevant information about a client's condition, the treatment provided, and the future course of action. Here’s a breakdown of each section:
Subjective (S): This section includes the client's own description of their condition, symptoms, and any relevant history. It often captures the client’s feelings, experiences, and complaints in their own words. For example:
"Client reports lower back pain after lifting heavy objects."
"Client feels tension in the shoulders and neck."
Objective (O): This section contains measurable and observable data gathered by the therapist. It includes physical findings, such as:
Range of motion measurements
Postural assessments
Palpable muscle tightness or tenderness
Assessment (A): This section is the therapist's professional evaluation of the client's condition based on the subjective and objective information. It may include:
Analysis of muscle imbalances
Identification of potential problem areas
Progress notes comparing previous sessions
Plan (P): This section outlines the treatment plan and any recommendations for the client. It includes:
Details of the massage techniques used
Frequency and duration of future sessions
Homework or self-care advice for the client
Using this S.O.A.P. notes template guarantees you will save time, cost and effort! It comes in PDF format, is ready to be tailored to your personal needs. Completing your document has never been easier!
Download this Massage Soap template now for your own benefit!
HAFTUNGSAUSSCHLUSS
Nichts auf dieser Website gilt als Rechtsberatung und kein Mandatsverhältnis wird hergestellt.
Wenn Sie Fragen oder Anmerkungen haben, können Sie sie gerne unten veröffentlichen.